Limitations of PGS
What you need to know about the limitations of PGS
Preimplantation genetic screening, or PGS, sounds like a dream come true for many people who hope to have an easy pregnancy and healthy child. While this advanced science does improve the chances of both, there are important limitations of PGS that hopeful parents need to understand.
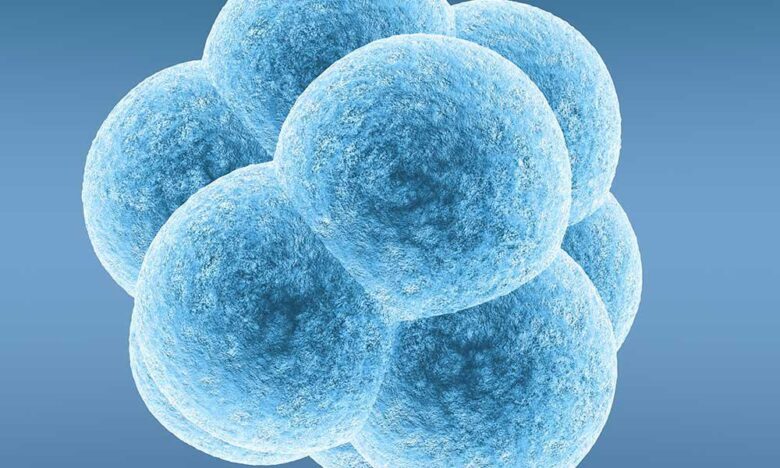
Before PGS became possible in the early 1980s, the only way to grade IVF embryos was to look at them under a microscope. Still, it’s been proven time and again that not all normal-looking embryos implant and grow into healthy babies, while countless low-grade embryos have grown into beautiful, healthy kids.
As the old saying goes, “You can’t judge a book by its cover.” With embryos, you have to take a look inside before you can tell if you’ve found a good one. PGS makes it possible for scientists to look inside an embryo and examine its genetic makeup so that the embryo with the best chance for growing into a healthy baby can be selected for transfer to the woman’s uterus.
In PGS, geneticists evaluate a few biopsied cells from each embryo for chromosomal aneuploidy, seeking to find out if too few or too many chromosomes are present. An embryo with more or fewer than 23 chromosome pairs may be at increased risk of miscarriage or certain genetic disorders.
By screening out abnormal embryos with PGS, physicians can transfer just one chromosomally normal embryo, increasing the chances for having a successful singleton pregnancy and healthy child. But it’s important to know the limitations of PGS because even when transferring a screened embryo the live birth rate is still just 60% or less.
Limitations of PGS: Why isn’t it foolproof?
In recent years, scientists have made many advances that have improved the accuracy and safety of PGS. Just a few years ago geneticists could evaluate only 10 chromosomes, allowing for 80% diagnostic accuracy. Today’s screening method allows evaluation of all 23 pairs of chromosomes at once, achieving accuracy greater than 98%.
Despite these advances, the initial enthusiasm about PGS has been tempered by more recent data. It’s become clear that maternal age plays an important role in live birth rates after PGS.
- The maximum post-PGS live birth rate for women younger than 35 is 60%.
- The live birth rate declines to 55% for women ages 35 to 40.
- For women ages 41 to 43 the live birth rate drops to 45%.
Why does a “normal” embryo from a 35-year-old woman have a better chance to survive than a “normal” embryo from a 40-year-old? The answer lies with a condition called mosaicism, which may become more likely to occur as women grow older.
Geneticists’ ability to screen for chromosomal abnormalities is limited by mosaicism, in which an embryo has two or more cell populations that have a different chromosomal makeup. Some of those cells may be abnormal, lowering the embryo’s potential for survival. But with current technologies, if fewer than 30% of an embryo’s cells are abnormal, those abnormalities may go undetected.
One of the limitations of PGS is that the sample size is small. Just four to 10 cells can be safely removed from an early-stage embryo without causing damage. If the biopsied cells are normal it doesn’t necessarily mean that every cell in the embryo is also normal. The embryo could be mosaic, and depending on the severity, it may be unable to develop normally after transfer.
If one or more of the biopsied cells is abnormal, that embryo will not be chosen for transfer. While healthy babies have been born from mosaic embryos – in one Italian study, the rate was 6 healthy babies out of 18 transfers – many fertility centers, including IVFMD, remain reluctant to transfer mosaic embryos until further safety studies have been done.
Talk to your fertility specialist
Since PGS was first introduced, science and technology have made great strides in helping people have healthy children. While embryo mosaicism remains one of the primary limitations of PGS, it’s just a matter of time until researchers find a way to overcome it.
If you’d like to learn more about PGS or have questions about genetic testing, contact us to schedule a consultation with the physicians at IVFMD.
- Special IVF Protocols for Diminished Ovarian Reserve - February 5, 2025
- Is IVF the Right Choice? - March 2, 2024
- What to Consider When Choosing a Fertility Clinic - February 29, 2024